Low Sperm Count – Symptoms And Causes
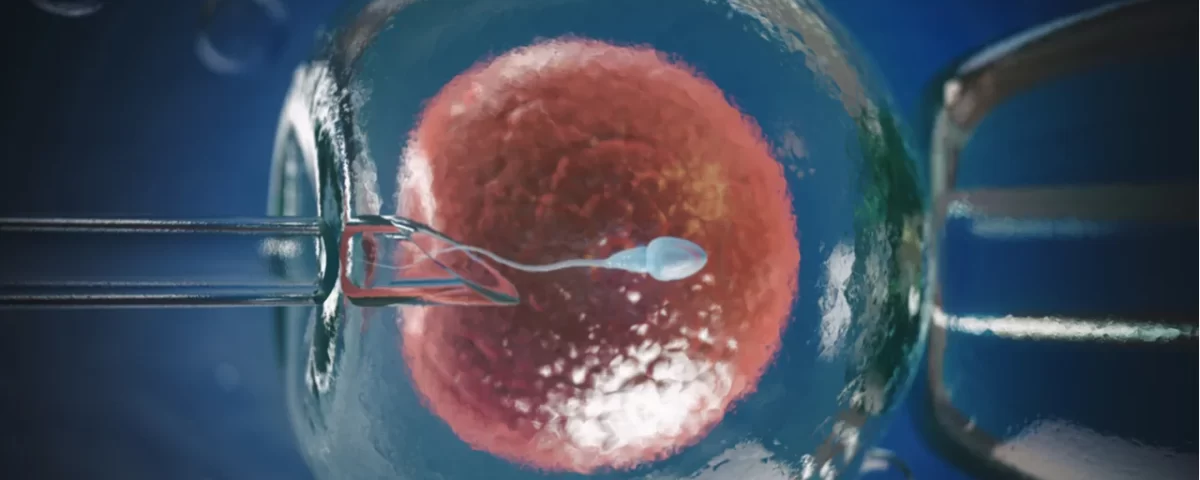
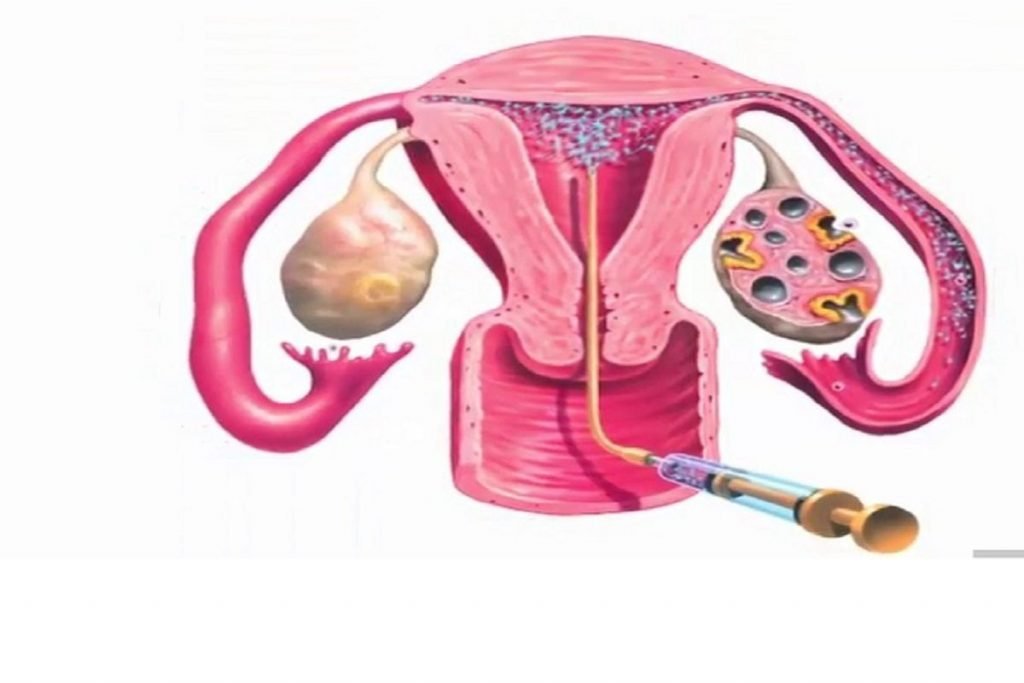
Low sperm count (oligospermia) means fewer than 15 million sperm per ml, and can range from mild (10–15 million/ml) to severe (less than 5 million/ml), while azoospermia means no sperm at all. It is a major cause of male infertility and often has no obvious symptoms beyond difficulty conceiving, though some men may notice low libido, erection issues, or testicular pain/changes. Common reasons include infections, varicocele, hormonal or genetic problems, undescended testes, certain surgeries, toxins, heat exposure, smoking, alcohol, drugs, obesity, and chronic illnesses. Evaluation usually involves detailed history, semen analysis, hormone tests, ultrasound, and sometimes genetic tests or testicular biopsy. Management can include treating infections or hormonal issues, surgery for blockages or varicocele, lifestyle changes, and using assisted reproductive techniques like IUI, IVF, or IVF-ICSI, sometimes with sperm retrieval directly from the testes or epididymis.